NIHR INCLUDE Impaired Capacity to Consent Framework
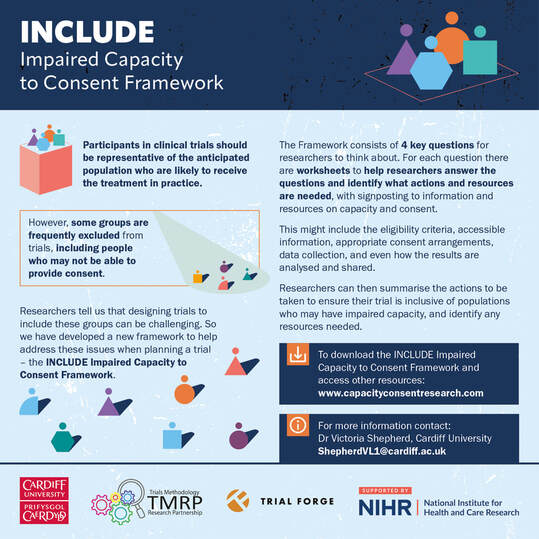
The NIHR INCLUDE Impaired Capacity to Consent Framework is a tool for researchers to ensure that their trial is designed to be inclusive of people with impaired capacity to consent, as well as improving the quality of the trial design and funding application. It should preferably be used at the earliest stage when designing a trial (for example, it might be used when developing an NIHR Stage 2 application), however it can also inform later stages of developing the trial such as when drafting the protocol and ethics application. The framework is intended to be used with all populations who may experience impaired capacity, although the issues raised will differ between populations and trial contexts..
The INCLUDE Impaired Capacity to Consent Framework has four key questions, each of which is intended to prompt trial teams to think about who should be included in the trial, and how to facilitate their involvement as much as possible. These questions should be considered by trial teams in partnership with patient and public partners.
Answering the key questions can be tricky. To help with this we have developed some worksheets that give pointers to the sort of things to think about when answering the questions. Not all questions/sections will be relevant and can be left out if they are not helpful. It is intended to be used for trials, but it may be useful for designing other types of studies – especially question 4 about whether the study design will affect inclusion.
The key questions and worksheets can be downloaded from the links below, together with a toolkit of resources to help researchers to use the Framework in practice. Lots of information and resources about conducting research involving adults with impaired capacity can be found under the resources tab on this website. You can find out more information about the project here.
The Framework was introduced at a webinar hosted by the Centre for Trials Research at Cardiff University, with a panel including Dr Victoria Shepherd, Prof Shaun Treweek, and Prof Paul Dark, and 350+ people registered to attend. A recording of the webinar can be viewed here, and the presentations can be accessed here.
The INCLUDE Impaired Capacity to Consent Framework has four key questions, each of which is intended to prompt trial teams to think about who should be included in the trial, and how to facilitate their involvement as much as possible. These questions should be considered by trial teams in partnership with patient and public partners.
Answering the key questions can be tricky. To help with this we have developed some worksheets that give pointers to the sort of things to think about when answering the questions. Not all questions/sections will be relevant and can be left out if they are not helpful. It is intended to be used for trials, but it may be useful for designing other types of studies – especially question 4 about whether the study design will affect inclusion.
The key questions and worksheets can be downloaded from the links below, together with a toolkit of resources to help researchers to use the Framework in practice. Lots of information and resources about conducting research involving adults with impaired capacity can be found under the resources tab on this website. You can find out more information about the project here.
The Framework was introduced at a webinar hosted by the Centre for Trials Research at Cardiff University, with a panel including Dr Victoria Shepherd, Prof Shaun Treweek, and Prof Paul Dark, and 350+ people registered to attend. A recording of the webinar can be viewed here, and the presentations can be accessed here.
Link to publication to cite: Shepherd V, Joyce K, Flynn S, Clout M, Lewis A, Nocivelli B, Segrott J, and Treweek S. Improving the inclusion of an under-served group in trials: development and implementation of the INCLUDE Impaired Capacity to Consent Framework. Trials 25, 83 (2024) https://doi.org/10.1186/s13063-024-07944-x
Help to use the INCLUDE Impaired Capacity to Consent Framework
If you are developing a funding application for a trial that includes (or should include) adults with impaired capacity to consent, we are offering up to 1.5 hours online discussion to help you apply the new INCLUDE Impaired Capacity to Consent Framework to your trial. Online discussions can be arranged at a time to suit. The trial team can refer to the trial having been designed using this framework in their application.
For more information about the INCLUDE Impaired Capacity to Consent Framework or to access this opportunity:
Please contact: Dr Victoria Shepherd
Email: [email protected]
Or via the contact page on this website
For more information about the INCLUDE Impaired Capacity to Consent Framework or to access this opportunity:
Please contact: Dr Victoria Shepherd
Email: [email protected]
Or via the contact page on this website
INCLUDE Impaired Capacity to Consent Framework
INCLUDE Framework document: four key questions and worksheetsDownload the four key questions and the worksheets as a single Word document, including a summary of the legal frameworks for research involving adults who lack capacity to consent (see the Appendix).
|
User guide for the INCLUDE FrameworkThis is a brief guide to using the INCLUDE Impaired Capacity to Consent Framework. It outlines the purpose of the Framework, how it was developed, when it should be used, and who should be involved in using the Framework.
|
Easy Read 'user guide' to the INCLUDE FrameworkThis accessible guide is intended to support public involvement when using the Framework. It introduces concepts such as capacity, informed consent, and clinical trials, in addition to providing information about the Framework. It was developed by Thinklusive.
|
Introduction to the INCLUDE Impaired Capacity to Consent Framework
Introductory infographicTwo page infographic style introduction to the INCLUDE Framework (Welsh language version also available)
|
Introductory flyerOne page infographic style flyer to raise awareness about the INCLUDE Framework (Welsh language version also available)
|
Explainer videoShort animated video of 2.5 mins to introduce the INCLUDE Framework (subtitles available, Welsh language version also available)
|
Library of worked examples of the INCLUDE Impaired Capacity to Consent Framework
We have prepared some worked examples of the Framework based on trials in a range of settings, populations, and contexts for impaired capacity, and involving different types of intervention. These examples are based on composite or actual trials and are intended to be illustrative rather than a definitive assessment of the trials. They were completed retrospectively by researchers who were not involved in the trial using publicly-accessible information. The aim is to add further examples to this library, therefore this resource will expand over time.
Example of a sepsis trialWorked example of an emergency trial which involves 'research without prior consent'
|
Example of a hip fracture trialWorked example of a trial of a a rehabilitation intervention for hip fracture management
|
Example of community-based trialWorked example of a trial of the management of a long-term urinary catheter in the community
|
FAQs about the INCLUDE Impaired Capacity to Consent Framework
We have developed a set of 'Frequently Asked Questions' based on questions raised during the launch webinar and feedback survey and when holding workshops with individual trial teams. The FAQs can be viewed and downloaded as a single file, or use the drop down questions below to view questions and responses individually.
Does the framework explain the different legal provisions across the different legal jurisdictions of the UK?
DOES THE FRAMEWORK EXPLAIN THE DIFFERENT LEGAL PROVISIONS ACROSS THE DIFFERENT LEGAL JURISDICTIONS OF THE UK?
The framework is designed to be generic across populations and settings. The legal frameworks governing research involving adults who lack capacity to consent vary across the different UK jurisdictions and by the type of research (i.e whether it is classified as a clinical trial of an investigational medicinal product or not). The introductory section of the framework signposts researchers to Appendix 1 which contains a summary of the requirements and terminology used in the different legal frameworks. This includes who is involved in decisions about adults who lack capacity to consent, how the decision should be made, and links to more information. Researchers are encouraged to review these prior to using the framework to design their study as these arrangements will need to be incorporated into the design.
Worksheet A also provides a reminder to consider whether the nature of participants’ capacity and how it might change over their time in the study, and to review the different legal frameworks accordingly using the summary in Appendix 1.
The impact of the different legal frameworks that researchers need to consider in their trial are threaded throughout the framework. Questions about the consent processes and documents that might be required are contained in Worksheet C, and questions about whether participants will remain in the study if capacity is lost during the study is contained in Worksheet E.
Throughout the framework researchers are signposted to the resources on this website which includes pages about the legal frameworks and how the requirements apply in different studies with downloadable summaries.
The framework is designed to be generic across populations and settings. The legal frameworks governing research involving adults who lack capacity to consent vary across the different UK jurisdictions and by the type of research (i.e whether it is classified as a clinical trial of an investigational medicinal product or not). The introductory section of the framework signposts researchers to Appendix 1 which contains a summary of the requirements and terminology used in the different legal frameworks. This includes who is involved in decisions about adults who lack capacity to consent, how the decision should be made, and links to more information. Researchers are encouraged to review these prior to using the framework to design their study as these arrangements will need to be incorporated into the design.
Worksheet A also provides a reminder to consider whether the nature of participants’ capacity and how it might change over their time in the study, and to review the different legal frameworks accordingly using the summary in Appendix 1.
The impact of the different legal frameworks that researchers need to consider in their trial are threaded throughout the framework. Questions about the consent processes and documents that might be required are contained in Worksheet C, and questions about whether participants will remain in the study if capacity is lost during the study is contained in Worksheet E.
Throughout the framework researchers are signposted to the resources on this website which includes pages about the legal frameworks and how the requirements apply in different studies with downloadable summaries.
Does the framework include guidance for emergency research conducted without prior consent?
DOES THE FRAMEWORK INCLUDE GUIDANCE FOR EMERGENCY RESEARCH CONDUCTED WITHOUT PRIOR CONSENT?
The framework is designed to be generic across populations and settings, including emergency and non-emergency research, although the issues that need to be considered will vary according to the context. The introductory section of the framework signposts researchers to Appendix 1 which contains a summary of the requirements used in the different legal frameworks, including research conducted in emergency situations which varies in different jurisdictions. Researchers are encouraged to review these prior to using the framework to design their study as these arrangements will need to be incorporated into the design.
The impact of the different legal frameworks that researchers need to consider in their trial are threaded throughout the framework. For example, questions about the consent processes and documents that might be required, including for emergency research conducted without prior consent, are contained in Worksheet C.
Worksheet E covers aspect of retention, including the ability for participants to remain in the trial if capacity is lost, whether data will be used if the team are unable to obtain retrospective/deferred consent or in event of death or withdrawal, and highlights that whether consent is considered to survive any loss of capacity depends on the relevant legal framework.
Throughout the framework researchers are signposted to the resources on this website which includes information about the legal frameworks and how the requirements apply to emergency research with links to resources including a patient video explaining ‘deferred consent’.
The framework is designed to be generic across populations and settings, including emergency and non-emergency research, although the issues that need to be considered will vary according to the context. The introductory section of the framework signposts researchers to Appendix 1 which contains a summary of the requirements used in the different legal frameworks, including research conducted in emergency situations which varies in different jurisdictions. Researchers are encouraged to review these prior to using the framework to design their study as these arrangements will need to be incorporated into the design.
The impact of the different legal frameworks that researchers need to consider in their trial are threaded throughout the framework. For example, questions about the consent processes and documents that might be required, including for emergency research conducted without prior consent, are contained in Worksheet C.
Worksheet E covers aspect of retention, including the ability for participants to remain in the trial if capacity is lost, whether data will be used if the team are unable to obtain retrospective/deferred consent or in event of death or withdrawal, and highlights that whether consent is considered to survive any loss of capacity depends on the relevant legal framework.
Throughout the framework researchers are signposted to the resources on this website which includes information about the legal frameworks and how the requirements apply to emergency research with links to resources including a patient video explaining ‘deferred consent’.
Does the framework apply differently to different trial phases, or different types of research studies?
DOES THE FRAMEWORK APPLY DIFFERENTLY TO DIFFERENT TRIAL PHASES, OR DIFFERENT TYPES OF RESEARCH STUDIES?
The framework is intended to be used to design clinical trials. However, we anticipate it is also useful when designing non-interventional studies and other types of research. The questions which specifically relate to the intervention or comparator (e.g Q2 and Q 3) may not be directly applicable but is likely that Q4 and Worksheets C-F which relate to the design aspects of the study will be widely applicable.
The framework is intended to be used to design clinical trials. However, we anticipate it is also useful when designing non-interventional studies and other types of research. The questions which specifically relate to the intervention or comparator (e.g Q2 and Q 3) may not be directly applicable but is likely that Q4 and Worksheets C-F which relate to the design aspects of the study will be widely applicable.
Should separate feasibility studies be carried out to understand if people who lack capacity to consent can not only be recruited, but are able to complete/adhere to the intervention?
SHOULD SEPARATE FEASIBILITY STUDIES BE CARRIED OUT TO UNDERSTAND IF PEOPLE WHO LACK CAPACITY TO CONSENT CAN NOT ONLY BE RECRUITED, BUT ARE ABLE TO COMPLETE/ADHERE TO THE INTERVENTION?
Inclusivity and diversity must be designed into studies from the outset. Feasibility studies play an important role in exploring whether aspects of the proposed trial design are feasible for the population concerned. This may include the intervention (if relevant and if it not already established in previous work) as well as recruitment and retention arrangements and data collection methods. Using the framework to design the feasibility study provides an opportunity to identify and explore feasibility issues around the intervention/comparator as well as those around recruitment and consent processes and data collection. Aspects of the trial can then be amended prior to designing and conducting a larger scale trial.
Worksheet A encourages researchers to consider how any factors relating to participants’ capacity-affecting condition or disability might influence their response to (or engagement with) the intervention/comparator.
Worksheet B enables researchers to consider how the intervention and/or comparator (including how they are provided), might make it harder for some groups in the population to respond to (or engage with) it. The factors listed in the worksheet are taken from the TIDieR guidelines for reporting interventions.
Worksheets C-F cover aspects of the trial design, including whether the data collection methods are appropriate and accessible for people with cognitive impairment who may encounter difficulties with self-reporting or whether alternative methods such as proxy reported outcomes are needed.
Inclusivity and diversity must be designed into studies from the outset. Feasibility studies play an important role in exploring whether aspects of the proposed trial design are feasible for the population concerned. This may include the intervention (if relevant and if it not already established in previous work) as well as recruitment and retention arrangements and data collection methods. Using the framework to design the feasibility study provides an opportunity to identify and explore feasibility issues around the intervention/comparator as well as those around recruitment and consent processes and data collection. Aspects of the trial can then be amended prior to designing and conducting a larger scale trial.
Worksheet A encourages researchers to consider how any factors relating to participants’ capacity-affecting condition or disability might influence their response to (or engagement with) the intervention/comparator.
Worksheet B enables researchers to consider how the intervention and/or comparator (including how they are provided), might make it harder for some groups in the population to respond to (or engage with) it. The factors listed in the worksheet are taken from the TIDieR guidelines for reporting interventions.
Worksheets C-F cover aspects of the trial design, including whether the data collection methods are appropriate and accessible for people with cognitive impairment who may encounter difficulties with self-reporting or whether alternative methods such as proxy reported outcomes are needed.
Do the worksheets provide guidance for working with relatives as personal consultees or personal legal representatives, or with staff members acting as nominated consultees or professional legal representatives?
DO THE WORKSHEETS PROVIDE GUIDANCE FOR WORKING WITH RELATIVES AS PERSONAL CONSULTEES OR PERSONAL LEGAL REPRESENTATIVES, OR WITH STAFF MEMBERS ACTING AS NOMINATED CONSULTEES OR PROFESSIONAL LEGAL REPRESENTATIVES?
The framework does not explicitly include guidance for working with consultees and legal representatives, but the questions raised in the framework enables researchers to consider who may need to be involved, how they might be identified and contacted, and what information documents should be developed for them.
The introductory section of the framework signposts researchers to Appendix 1 which contains a summary of the arrangements for identifying and involving consultees and legal representatives which varies in different jurisdictions and links for more information about how to work with them (e.g MCA Code of Practice and Guidance on Nominating a Consultee). Researchers are encouraged to review these prior to using the framework to design their study as these arrangements will need to be incorporated into the design.
Throughout the framework researchers are signposted to the resources on this website which includes information about the legal frameworks and how consultees and legal representatives are involved. The website also contains a publications page with studies reporting the experiences of relatives acting as consultees/legal representatives and an analysis of information sheets provided to personal and professional consultees/legal representatives. This may help researchers to understand consultees/legal representatives’ informational and decisional needs.
The framework does not explicitly include guidance for working with consultees and legal representatives, but the questions raised in the framework enables researchers to consider who may need to be involved, how they might be identified and contacted, and what information documents should be developed for them.
The introductory section of the framework signposts researchers to Appendix 1 which contains a summary of the arrangements for identifying and involving consultees and legal representatives which varies in different jurisdictions and links for more information about how to work with them (e.g MCA Code of Practice and Guidance on Nominating a Consultee). Researchers are encouraged to review these prior to using the framework to design their study as these arrangements will need to be incorporated into the design.
Throughout the framework researchers are signposted to the resources on this website which includes information about the legal frameworks and how consultees and legal representatives are involved. The website also contains a publications page with studies reporting the experiences of relatives acting as consultees/legal representatives and an analysis of information sheets provided to personal and professional consultees/legal representatives. This may help researchers to understand consultees/legal representatives’ informational and decisional needs.
Does the framework provide any guidance on retention in trials when including those with impaired capacity to consent?
DOES THE FRAMEWORK PROVIDE ANY GUIDANCE ON RETENTION IN TRIALS WHEN INCLUDING THOSE WITH IMPAIRED CAPACITY TO CONSENT?
Capacity can fluctuate over for time, and some participants' capacity status may change during their time in a trial (i.e they may regain or lose capacity). This might be particularly anticipated in some populations or settings, and where a longer follow up period is planned. Prospectively planning for these situations will avoid amendments to the trial design (and so seek approvals for these amendments) at a later point and reduce loss to follow up.
The summary of the legal frameworks in Appendix 1 includes the different arrangements for loss of capacity during research.
Worksheet E encourages researchers to consider whether participants are able to remain in the trial if capacity is lost, and about the use of data if the participant dies (including if the research team are unable to obtain consent for participants enrolled without prior consent or where a professional has acted as a consultee or legal representative). A range of information sheets to reflect these changes in consent arrangements will be needed (e.g a ‘regained capacity’ information sheet to reflect that the participant is agreeing to remain in the study rather than providing consent at the outset).
The framework signposts to the resources on this website for more information about the legal frameworks and how they govern the loss and regaining of capacity, including the page on ‘research conduct’.
Capacity can fluctuate over for time, and some participants' capacity status may change during their time in a trial (i.e they may regain or lose capacity). This might be particularly anticipated in some populations or settings, and where a longer follow up period is planned. Prospectively planning for these situations will avoid amendments to the trial design (and so seek approvals for these amendments) at a later point and reduce loss to follow up.
The summary of the legal frameworks in Appendix 1 includes the different arrangements for loss of capacity during research.
Worksheet E encourages researchers to consider whether participants are able to remain in the trial if capacity is lost, and about the use of data if the participant dies (including if the research team are unable to obtain consent for participants enrolled without prior consent or where a professional has acted as a consultee or legal representative). A range of information sheets to reflect these changes in consent arrangements will be needed (e.g a ‘regained capacity’ information sheet to reflect that the participant is agreeing to remain in the study rather than providing consent at the outset).
The framework signposts to the resources on this website for more information about the legal frameworks and how they govern the loss and regaining of capacity, including the page on ‘research conduct’.
Do you have examples of completed FRAMEWORKS used in other studies to look at?
DO YOU HAVE EXAMPLES OF COMPLETED FRAMEWORKS USED IN OTHER STUDIES TO LOOK AT?
Yes, the section above on this website has a library of completed frameworks that can be used as a reference. This includes trials in a range of settings, populations, and contexts, and involving different types of intervention. The intention is to expand this resource and we are keen to hear from researchers about any particular types of trials/populations they would like to be included, or if they would like to contribute their completed frameworks to the library (they can be anonymised if preferred).
Yes, the section above on this website has a library of completed frameworks that can be used as a reference. This includes trials in a range of settings, populations, and contexts, and involving different types of intervention. The intention is to expand this resource and we are keen to hear from researchers about any particular types of trials/populations they would like to be included, or if they would like to contribute their completed frameworks to the library (they can be anonymised if preferred).
When and how should a potential participant's capacity to consent be assessed? Is consent required prior to conducting a capacity assessment ?
WHEN AND HOW SHOULD A POTENTIAL PARTICIPANT'S CAPACITY TO CONSENT BE ASSESSED? IS CONSENT REQUIRED PRIOR TO CONDUCTING A CAPACITY ASSESSMENT?
Mental capacity legislation has a number of underpinning principles. There is a legal presumption that a person has capacity to make a decision, unless there are concerns otherwise. Capacity is time and decision-specific, and so a person may have capacity to make some decisions and not others. If there are concerns that someone lacks capacity to consent to a study, there may be steps that can be taken to support the person to make their own decisions e.g to delay the decision until they regain capacity or to provide supported decision-making. The resources on this website includes information about the process of assessing capacity and about supported decision-making.
Questions about consent and capacity assessment processes are contained in Worksheet C. If indicated, a capacity assessment should be carried out by the person who requires the decision to be made (e.g the member of the research team who is seeking consent) and documented. Those involved in caring for the person may be able to advise the researcher about the person’s communication and capacity needs. ‘Consent’ is not required before an assessment of the person’s capacity is carried out, where it forms part of the process for recruiting participants. If the person is receiving care in a setting such as a care home for example, the care staff may introduce the researcher to them.
Mental capacity legislation has a number of underpinning principles. There is a legal presumption that a person has capacity to make a decision, unless there are concerns otherwise. Capacity is time and decision-specific, and so a person may have capacity to make some decisions and not others. If there are concerns that someone lacks capacity to consent to a study, there may be steps that can be taken to support the person to make their own decisions e.g to delay the decision until they regain capacity or to provide supported decision-making. The resources on this website includes information about the process of assessing capacity and about supported decision-making.
Questions about consent and capacity assessment processes are contained in Worksheet C. If indicated, a capacity assessment should be carried out by the person who requires the decision to be made (e.g the member of the research team who is seeking consent) and documented. Those involved in caring for the person may be able to advise the researcher about the person’s communication and capacity needs. ‘Consent’ is not required before an assessment of the person’s capacity is carried out, where it forms part of the process for recruiting participants. If the person is receiving care in a setting such as a care home for example, the care staff may introduce the researcher to them.
Is there commitment from funders to provide additional funding to enable researchers to include all populations who might benefit from the research as inclusive trials may be more costly?
IS THERE COMMITMENT FROM FUNDERS TO PROVIDE ADDITIONAL FUNDING TO ENABLE RESEARCHERS TO INCLUDE ALL POPULATIONS WHO MIGHT BENEFIT FROM THE RESEARCH AS INCLUSIVE TRIALS MAY BE MORE COSTLY?
Some of the actions identified when designing a trial to be inclusive of adults with impaired capacity may require additional resources or costs. Many funders are committed to increasing inclusivity and diversity in research as a strategic priority. A number of funders signpost applicants to the INCLUDE frameworks (some are listed on the Trial Forge website). The use of this (and other) frameworks when developing a funding application can help to build in costs associated with inclusivity from the outset, and to provide justification to the funders about what these costs are and why they have been included.
Some of the actions identified when designing a trial to be inclusive of adults with impaired capacity may require additional resources or costs. Many funders are committed to increasing inclusivity and diversity in research as a strategic priority. A number of funders signpost applicants to the INCLUDE frameworks (some are listed on the Trial Forge website). The use of this (and other) frameworks when developing a funding application can help to build in costs associated with inclusivity from the outset, and to provide justification to the funders about what these costs are and why they have been included.
It seems like the framework would need to be used at the outset, and then reviewed often and updated when appropriate. What advice is there for busy trial teams who already have so much going on?
IT SEEMS LIKE THE FRAMEWORK WOULD NEED TO BE USED AT THE OUTSET, AND THEN REVIEWED OFTEN AND UPDATED WHEN APPROPRIATE. WHAT ADVICE IS THERE FOR BUSY TRIAL TEAMS WHO ALREADY HAVE SO MUCH GOING ON?
The framework does take time to work through and should be done collaboratively – including with patient and public contributors – at the earliest stage of developing a trial. Issues around inclusion of groups such as those with impaired capacity to consent can be complex, however considering any barriers and how to address them is likely to improve the quality of the funding application, increase the usefulness of the trial results, and save time later in the trial development process as many of the issues will have been considered prospectively. Responses to the questions can then be revisited when developing the protocol and other documentation for the trial.
The summary of actions and resources identified in Worksheet G can be added to the ‘justification of costs’ section of the funding application.
Responses to Q1 about why the trial should include people with impaired capacity can be used in the IRAS form section about why the trial cannot only be conducted with people who can provide their own consent when applying for ethical approval.
The consent documents and processes outlined in Worksheet C (including who is involved, what documents are required, and what happens if capacity changes over time) can also be used in the ethics application and when developing participant documents for the trial.
The framework does take time to work through and should be done collaboratively – including with patient and public contributors – at the earliest stage of developing a trial. Issues around inclusion of groups such as those with impaired capacity to consent can be complex, however considering any barriers and how to address them is likely to improve the quality of the funding application, increase the usefulness of the trial results, and save time later in the trial development process as many of the issues will have been considered prospectively. Responses to the questions can then be revisited when developing the protocol and other documentation for the trial.
The summary of actions and resources identified in Worksheet G can be added to the ‘justification of costs’ section of the funding application.
Responses to Q1 about why the trial should include people with impaired capacity can be used in the IRAS form section about why the trial cannot only be conducted with people who can provide their own consent when applying for ethical approval.
The consent documents and processes outlined in Worksheet C (including who is involved, what documents are required, and what happens if capacity changes over time) can also be used in the ethics application and when developing participant documents for the trial.
The INCLUDE Impaired Capacity to Consent Framework was developed by members of the Inclusivity theme sub-group of the MRC-NIHR TMRP Trial Conduct Working Group. See the Acknowledgements section of the Framework for a full list of contributors. It is supported by the National Institute for Health and Care Research (NIHR) INCLUDE initiative and Trial Forge. The implementation of the INCLUDE Impaired Capacity to Consent Framework was funded by a Cardiff University Innovation for All award. CONSULT is funded by the Welsh Government through Health and Care Research Wales.